There’s something that doesn’t get talked about enough in recovery circles—what it feels like years after treatment.
When you’re newly sober, everything feels fragile and urgent. Your tools are fresh in your hands. You lean on structure, routine, community, and the rhythm of daily check-ins like your life depends on it—because, at the time, it probably did.
But then, time passes.
You stabilize. You build a life. The chaos shrinks. And without realizing it, you begin to wonder if you’re still even “in recovery”—or if you’re just… living.
Then comes the drift.
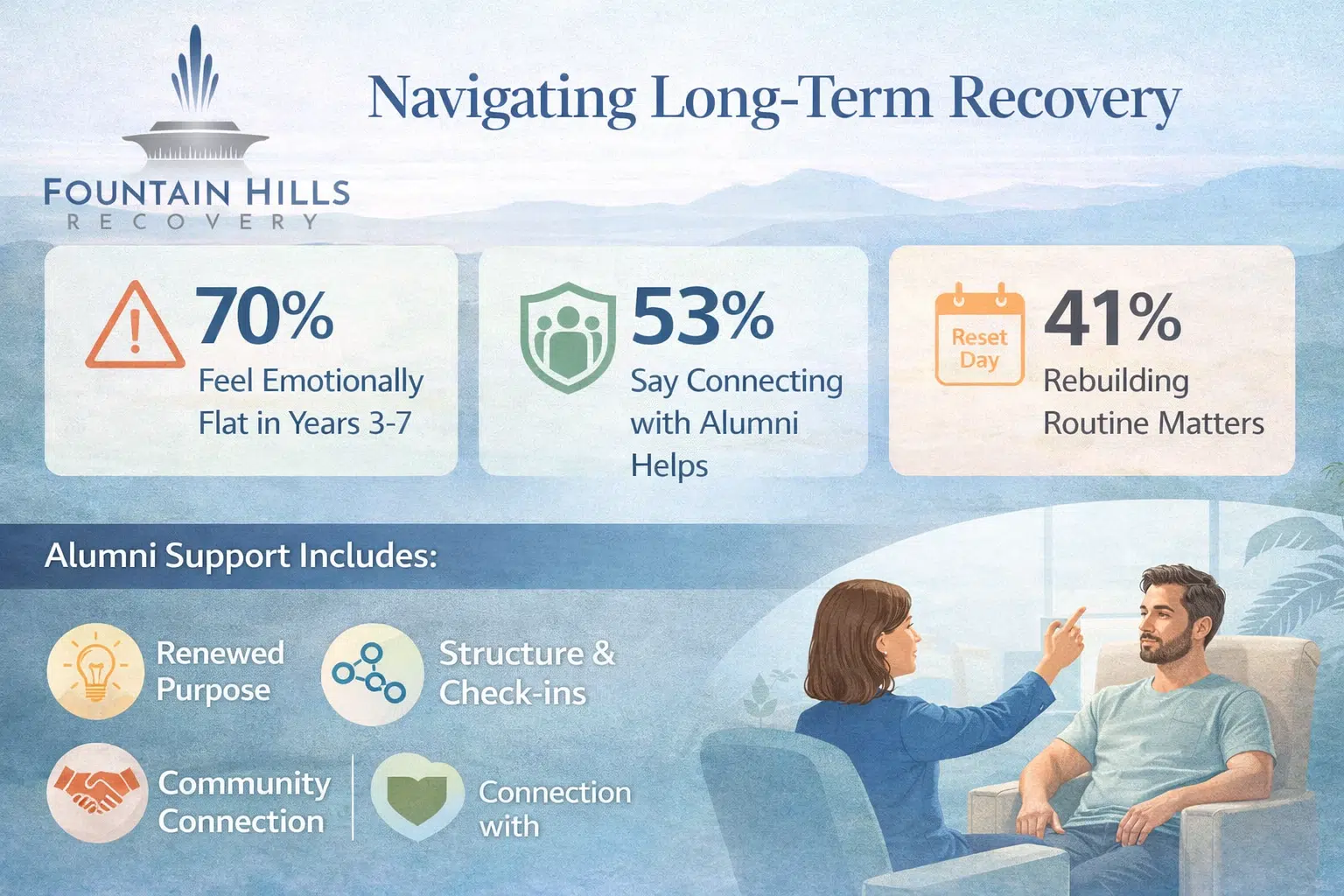
Not a relapse. Not even cravings. But something subtler. A sense of flatness. Disconnection. Emotional distance from the very tools that once saved you.
If that’s where you are, you’re not failing. You’re evolving.
At Fountain Hills Recovery, we work with alumni who’ve experienced exactly this. People who left inpatient drug rehab equipped and hopeful—only to find themselves, years later, wondering how to reconnect with what once felt vital.
This blog is a reflection of those conversations. A reminder that the tools you took with you still matter—and that you’re allowed to return to them without guilt, shame, or starting over.
Recovery tools aren’t expiration dated
Many alumni describe the tools they learned in inpatient treatment as “first aid” for early sobriety. Emergency breathing techniques. Crisis planning. Step work. Reaching out instead of isolating.
In early recovery, those tools were your armor.
Now, maybe they’re gathering dust. Or they feel too elementary for where you are. That doesn’t mean they’re useless. It just means your context has changed.
One client described it this way:
“I used to journal to process triggers. Now I journal to spot burnout before it takes over my week.”
The same tool. Different purpose.
Long-term recovery often means relearning how to use your early tools in ways that match your current life. The need isn’t gone—it’s just quieter.
Structure still helps—especially when you don’t “need” it
Inpatient drug rehab gave many of us structure by default. Wake-up times. Group therapy. Meal windows. Reflection blocks. That rhythm held you when you didn’t know how to hold yourself.
Today, you might not have that scaffolding. Your life may be flexible, busy, unpredictable. And while that might feel like progress, it can also lead to drift.
We’ve seen alumni rekindle structure by:
- Blocking out a solo walk every Sunday with no phone, just reflection
- Setting a monthly “reset day” to clean their space, look at goals, and reconnect
- Creating a personal check-in form—a simple journal page with three questions: How’s my body? How’s my mind? What do I need?
Structure doesn’t need to be rigid. It just needs to hold you when you forget to hold yourself.
Support systems evolve—but shouldn’t vanish
Remember the early days—when you had a sponsor’s number saved as a favorite? When your group chat buzzed with daily check-ins?
Over time, those systems fade. Not because you don’t need people, but because life gets loud. But when disconnection replaces community, even subtle loneliness can grow roots.
Long-term alumni often say, “I didn’t realize how alone I’d become until I tried to name someone I could call.”
That realization doesn’t mean you’re isolated. It means it’s time to rebuild—with less urgency, but the same intention.
This could look like:
- Reconnecting with alumni from your program (they probably feel the same way)
- Finding a therapist who understands long-term recovery—not just crisis mode
- Starting a monthly dinner, Zoom call, or message thread with someone who gets it
Your recovery doesn’t have to be loud or public. But it does have to be supported.
Emotional flatness is not failure—it’s information
There’s a tricky season in recovery where things are “fine”—but you’re numb. Not depressed. Not in danger. Just… low on fire. You go through the motions, but the deeper sense of purpose you once had feels muted.
This is especially common in years 3–7 post-treatment. By then, you’ve likely checked the major boxes: sobriety, housing, stability, relationships. What no one warned you about is how empty that can feel if your inner life hasn’t caught up.
That flatness doesn’t mean you’re ungrateful or broken. It means your soul is asking for attention.
This might be the time to:
- Revisit values work you did in treatment and see what’s changed
- Get curious about new forms of spiritual, creative, or emotional practice
- Reframe recovery as growth—not just maintenance
You’re not lost. You’re ready to expand.
Revisiting treatment doesn’t mean starting over
We’ve had alumni return to us years later—not because they relapsed, but because they felt off-course.
Sometimes, that looks like joining a week-long alumni intensive. Sometimes it’s a single call with a former therapist. Sometimes it’s stepping into a new program—like trauma work they weren’t ready for in early sobriety.
Coming back isn’t failure. It’s maturity. It says: I know myself well enough to ask for help before I fall.
If inpatient drug rehab gave you the language to recover, returning can give you the depth to evolve.
What “tools” actually look like 5, 10, 15 years later
They look different—but they’re still tools.
We’ve seen alumni use their recovery wisdom in new ways:
- A parent who adapted their relapse prevention plan into a framework for parenting teens with boundaries and empathy
- A business owner who revisits the “HALT” acronym weekly to check in with her team and herself
- A musician who transformed nightly prayer into a daily songwriting ritual—a space to release emotion without shame
Recovery doesn’t end. It reinvents itself.
And the person you are today might need to hear something you wrote to yourself back then. Open the notebook. Look again.
FAQs: Long-Term Recovery and Staying Grounded Years After Inpatient Rehab
Is it normal to feel “off” even when life looks good?
Yes. Emotional plateaus are part of long-term recovery. Just because you’re not in crisis doesn’t mean you don’t need support or reconnection.
Should I be worried if I haven’t used my recovery tools in a while?
Not necessarily. Life shifts. Your tools may have gone quiet, but that doesn’t mean they’re gone. Start by noticing what feels flat or heavy—then ask what tool used to help with that. You’re allowed to bring it back.
Can I come back to treatment if I haven’t relapsed?
Absolutely. Many alumni return for refreshers, new goals, trauma work, or emotional clarity—not just relapse prevention. Recovery isn’t linear. And support isn’t conditional.
I’m not in touch with anyone from rehab. How do I reconnect?
Start small. Reach out to your treatment center—they may have alumni groups or events. Consider therapy as a safe place to re-enter the recovery conversation. You don’t need to go back in time. You just need to take one step forward.
Long-term recovery isn’t about getting it perfect. It’s about staying real. And if “real” right now feels disconnected, numb, or uncertain—you’re not alone.
You don’t have to rebuild from scratch. You just have to remember what already helped you grow. And let it help you again, in a new way.
Reconnect with the inpatient drug rehab team in Fountain Hills that first helped you get grounded. Your next season of growth deserves just as much care as your first.
Call (800) 715-2004 or visit Inpatient Drug Rehab in Fountain Hills, AZ to learn more about how we support alumni at every stage—from restart to reconnection.